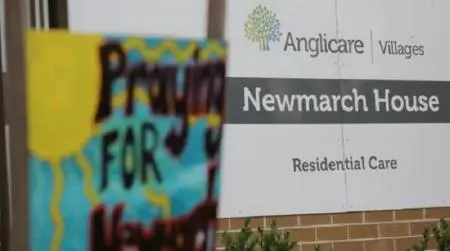
AT the time of writing, 63 nursing home residents had been infected with coronavirus. Of those, 26 had died and of those who died 17 lived in Newmarch House in Penrith.
Newmarch House had a good reputation locally before it was hit by the virus.
The aged care watchdog intervened twice in Newmarch before forcing the home to appoint an “Independent Adviser”. Prior to that, the watchdog had put in “a team experienced in managing COVID-19”.
The watchdog did not explain what an Independent Adviser was going to do what “a team experienced in managing COVID-19” couldn’t do. The appointed person turned out to have no clinical experience.
Newmarch House also won’t be able to admit any new residents as part of the penalty applied to it.
This is a most ridiculous penalty.
Who would go live in Newmarch now?
Or rather, who would go and live in any nursing home now?
Even the nursing home industry itself is beginning to realise it might be in trouble. Mike Rungie, a veteran of the industry, said that “occupancy was dropping in both residential and home care suggesting that some older people don’t think it’s safe”.
In fact, the Australian Government has hastily amended the Aged Care Act to allow residents to be taken out of a nursing home without that person having to keep paying fees while they wait out coronavirus living with family.
In May, an unprepared industry hastily put together an Industry Code for Visiting Residential Aged Care Homes. This was three months after the coronavirus had landed in Australia.
Meanwhile, nursing homes had done what they always do when an infectious disease strikes them: lock down completely.
Only, coronavirus outbreaks are not gastro outbreaks, which last only a short time.
Many nursing homes did little or nothing to prepare for the arrival of the coronavirus in Australia.
The Australian Nurses and Midwives Federation (ANMF) surveyed 2,000 of its members working in aged care.
Only 40 per cent of respondents said the nursing home they worked in was prepared for a COVID-19 outbreak, and less than 30 per cent said their home had enough supplies of Personal Protective Equipment (PPE).
While 77 per cent of respondents’ employers had recently updated or implemented infection control procedures for staff, almost a quarter of homes had done nothing in this regard.
But it gets even more outrageous than that.
The ongoing tragedy at Newmarch House demonstrated how essential it is to have good infection control procedures and to have sufficient, qualified staff to apply them. Yet the aged care provider peak organisation Leading Aged Services Australia (LASA), with much fanfare, introduced a newly created Aged Care Assistant role.
This role is junior to the Assistant in Nursing role, which is much criticised as requiring only the skimpiest of professional qualifications.
Anyone can apply to become an Aged Care Assistant and after a successful interview, you will do a 10-hour course, consisting of no less than nineteen modules.
Then you will be let loose in a nursing home.
It is very obvious that the relatively low coronavirus infection rate in Australian nursing homes is down to luck, not skill. And the luck consists in the success that Australian Governments have had in suppressing infection rates generally and nationally.
There would be many Newmarch Houses all over the country otherwise.